Can Diabetes Be Cured Permanently? Truth, Treatments, and Natural Management
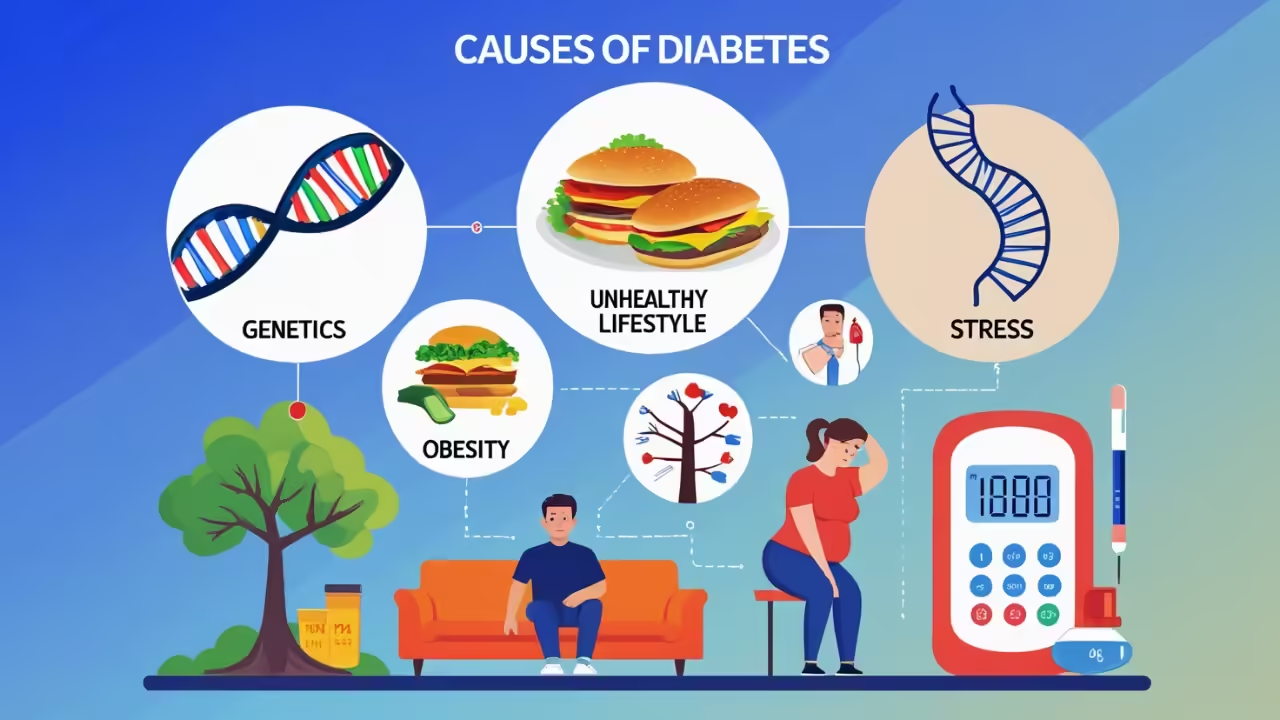
Can Diabetes Be Cured Permanently? Truth, Treatments, and Natural Management Understanding Diabetes Diabetes is a chronic condition that affects how the body regulates blood sugar (glucose) levels. Glucose is the primary source of energy for cells, and insulin, a hormone produced by the pancreas, helps transport glucose into the cells. When insulin is insufficient