The Role of the Immune System in Type 1 Diabetes | Autoimmune Insights & Research
Type 1 diabetes( T1D) is further than just a blood sugar problem — it’s a condition where the body’s vulnerable system turns snake, launching an attack against its own insulin- producing cells. Unlike Type 2 diabetes, which is often linked to lifestyle factors, T1D is classified as an autoimmune disease, arising when the immune system mistakenly targets the pancreas, specifically the beta cells responsible for insulin production. In this article, we’ll explore The Role of the Immune System in Type 1 Diabetes, delve into the mechanisms of this internal sabotage, and look at what current diabetes research reveals about future treatments and prevention.
Understanding Autoimmune Disease: The Basics of Self-Sabotage
The human immune system is a complex defense network designed to protect the body from harmful pathogens like viruses and bacteria. Still, in autoimmune conditions, this same system misidentifies the body’s own apkins as pitfalls. In Type 1 diabetes, the target is the beta cells in the pancreas. These cells play a crucial role in regulating blood sugar levels by producing insulin, a hormone that allows cells to absorb glucose from the bloodstream for energy.
The exact trigger of this autoimmune response remains one of the unsolved puzzles in diabetes research. Genetic predisposition combined with environmental factors—such as viral infections—are thought to initiate the autoimmune process. Over time, the vulnerable system’s grim attack destroys beta cells, leading to a near-complete halt in insulin product. Once insulin is gone, glucose remains in the bloodstream, causing dangerously high blood sugar levels, the hallmark of Type 1 diabetes.
Your Ultimate Klinio Diet Sample Menu: A Balanced Approach to Managing Diabetes
The Immune Attack: How Beta Cells Become Enemy Targets
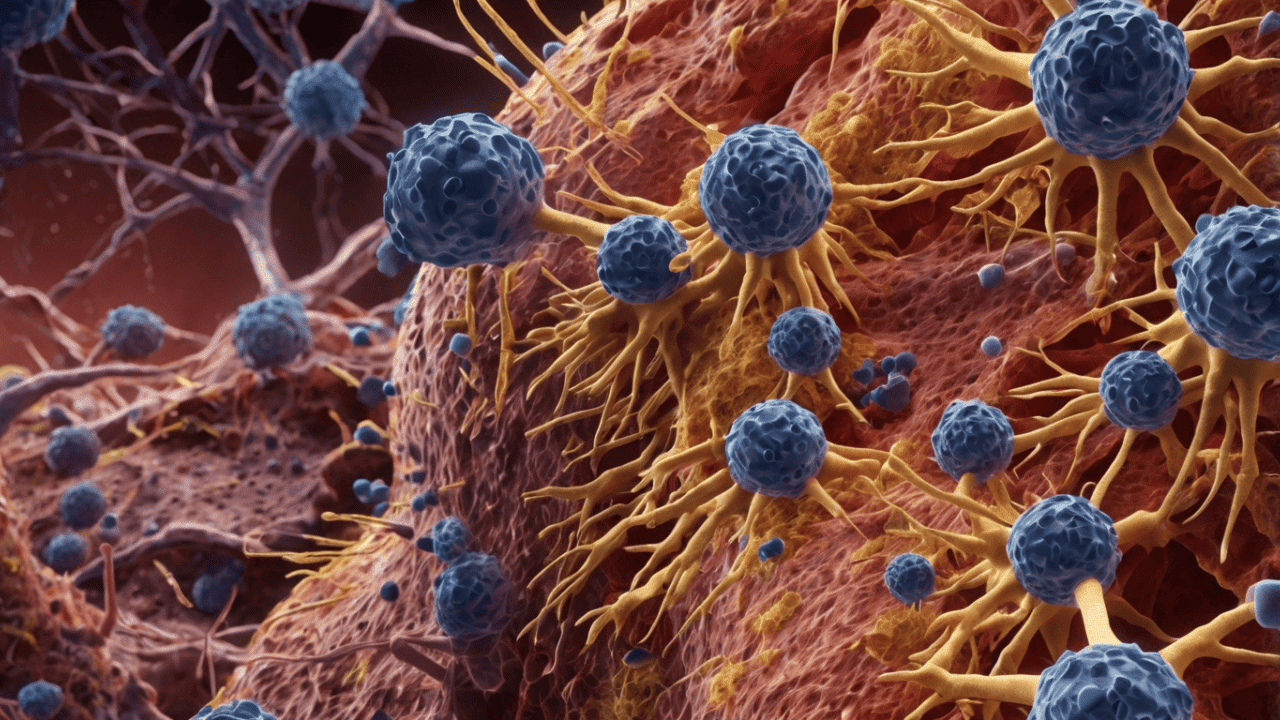
So what exactly goes wrong in the immune system? In people with Type 1 diabetes, immune cells such as T lymphocytes become overly aggressive. Instead of distinguishing between foreign invaders and self-tissue, they begin to identify the body’s own pancreatic beta cells as foreign. This breakdown in immune tolerance is central to the pathology of T1D.
One theory is that molecular mimicry—where a virus shares similar molecular patterns with beta cells—may trick the immune system into targeting both. Another theory points to a flaw in how the immune system is educated during early development, potentially allowing self-reactive T cells to escape deletion. Anyhow of the cause, the outgrowth is the same an vulnerable attack on the pancreas, leading to unrecoverable damage and loss of insulin- producing function.
Markers such as autoantibodies often appear years before symptoms, offering a glimpse into the early autoimmune process. These include insulin autoantibodies (IAA), GAD65, and IA-2. Their presence helps identify individuals at high risk and opens the door to preventive strategies, a major focus of ongoing diabetes research.
Consequences of the Immune Destruction: Life Without Insulin
Without insulin, the body’s metabolism unravels. Glucose accumulates in the bloodstream because cells can no longer absorb it. This condition, known as hyperglycemia, is the defining feature of Type 1 diabetes. Over time, consistently high blood sugar levels can lead to a cascade of complications affecting nearly every organ system.
Short-term consequences include diabetic ketoacidosis (DKA), a life-threatening condition where the body begins to break down fat for energy, producing toxic ketones. Long-term effects include nerve damage, kidney disease, blindness, and cardiovascular issues.
Since the pancreas can no longer regulate insulin production, individuals with T1D must manage their condition manually through daily insulin injections or insulin pumps. Even with tight glucose monitoring, replicating the body’s natural glucose-insulin balance remains a challenge. This constant vigilance underscores the urgent need for therapies that address the autoimmune component of the disease, not just its symptoms.
Diabetes Causes and Risk Factors: Genetic and Environmental Triggers
While the immune attack is the immediate cause of Type 1 diabetes, understanding what initiates that immune dysfunction is crucial for prevention. Genetics play a significant role—certain HLA genes on chromosome 6 are strongly linked to T1D susceptibility. However, genetics alone don’t tell the full story, as not all individuals with high-risk genes develop the disease.
Environmental factors are thought to trigger the autoimmune cascade. These may include viral infections like enteroviruses, dietary components such as cow’s milk proteins introduced early in life, and even gut microbiota imbalances. Geographic trends also suggest that colder climates and less sun exposure, which can affect vitamin D levels, may influence disease development.
Researchers continue to explore these diabetes causes, aiming to piece together how and why the immune system goes rogue. The goal is to identify modifiable risk factors and develop interventions to halt the autoimmune process before it leads to full-blown Type 1 diabetes.
Frontiers in Diabetes Research: Immunotherapy and Beyond
Modern diabetes research is shifting its focus from symptom management to immune modulation. Scientists are now exploring ways to halt or reverse the autoimmune attack at its root. Immunotherapy, long used in cancer treatment, is showing promise in altering the immune response in T1D.
Drugs like teplizumab—a monoclonal antibody—have been shown to delay the onset of Type 1 diabetes in high-risk individuals by interfering with the activation of aggressive T cells. Other approaches involve re-educating the immune system to tolerate beta cells again, using vaccines or cell-based therapies.
Stem cell research is also gaining momentum, aiming to regenerate lost beta cells or transplant lab-grown insulin-producing cells. Combined with encapsulation technologies that protect these cells from immune attack, such therapies could one day provide a functional cure.
innovations highlight a paradigm shift: treating the root immune dysfunction, not just the symptoms. While not yet mainstream, they represent hope for millions living with or at risk of T1D.
Conclusion: Turning the Tide in the Fight Against Type 1 Diabetes
The function of the immune system in Type 1 Diabetes is both crucial and intricate. This autoimmune disease represents a misfire of the body’s most sophisticated defense system, resulting in the destruction of insulin-producing beta cells and lifelong dependency on insulin therapy. While genetics and environment lay the groundwork, it is the immune system’s misguided attack that seals the diagnosis.
However, the future looks promising. With cutting-edge diabetes research exploring immune modulation, beta cell regeneration, and early diagnostics, the day may come when we can prevent or even cure Type 1 diabetes. Until then, understanding the immune mechanics behind the disease is our best defense—and our best hope.
FAQs About The Role of the Immune System in Type 1 Diabetes
- What is the role of the immune system in Type 1 diabetes?
In Type 1 diabetes, the immune system mistakenly attacks the insulin-producing beta cells in the pancreas. This autoimmune response destroys the cells responsible for insulin production, leading to high blood sugar levels and lifelong insulin dependence.
- How is Type 1 diabetes classified as an autoimmune disease?
Type 1 diabetes is considered an autoimmune disease because it is caused by the immune system’s abnormal response against the body’s own tissues—specifically, the beta cells in the pancreas. The body treats these cells as if they were harmful invaders.
- What causes the immune system to attack beta cells?
The exact cause is unknown, but diabetes research suggests a combination of genetic susceptibility and environmental triggers, such as viral infections or early diet. Dysregulation of the immune system and an eventual assault on pancreatic beta cells may result from these circumstances.
- Is it possible to prevent or reverse the immunological onslaught in people with Type 1 diabetes?
Immunotherapy is one of the new diabetes treatments that aims to prevent or postpone the immunological onslaught. Some experimental therapies have shown promise in preserving remaining beta cell function, but a full reversal is not yet widely available.
- How is insulin production affected in Type 1 diabetes?
Insulin production is severely reduced or completely halted in people with Type 1 diabetes due to the destruction of beta cells by the immune system. As a result, external insulin therapy is required to manage blood sugar levels.
- What are the early signs of immune system dysfunction in diabetes?
Early signs include the presence of autoantibodies targeting beta cells, which can appear years before any symptoms. At this stage, individuals may not show any signs of high blood sugar but are at high risk for developing Type 1 diabetes.
- Are there any preventive strategies for Type 1 diabetes?
As of right now, Type 1 diabetes cannot be prevented. However, research is exploring immune-modulating drugs, vaccines, and early screening in genetically at-risk individuals to delay or prevent the onset of the disease.