What Is Diabetes: Understanding Causes, Types, and Management
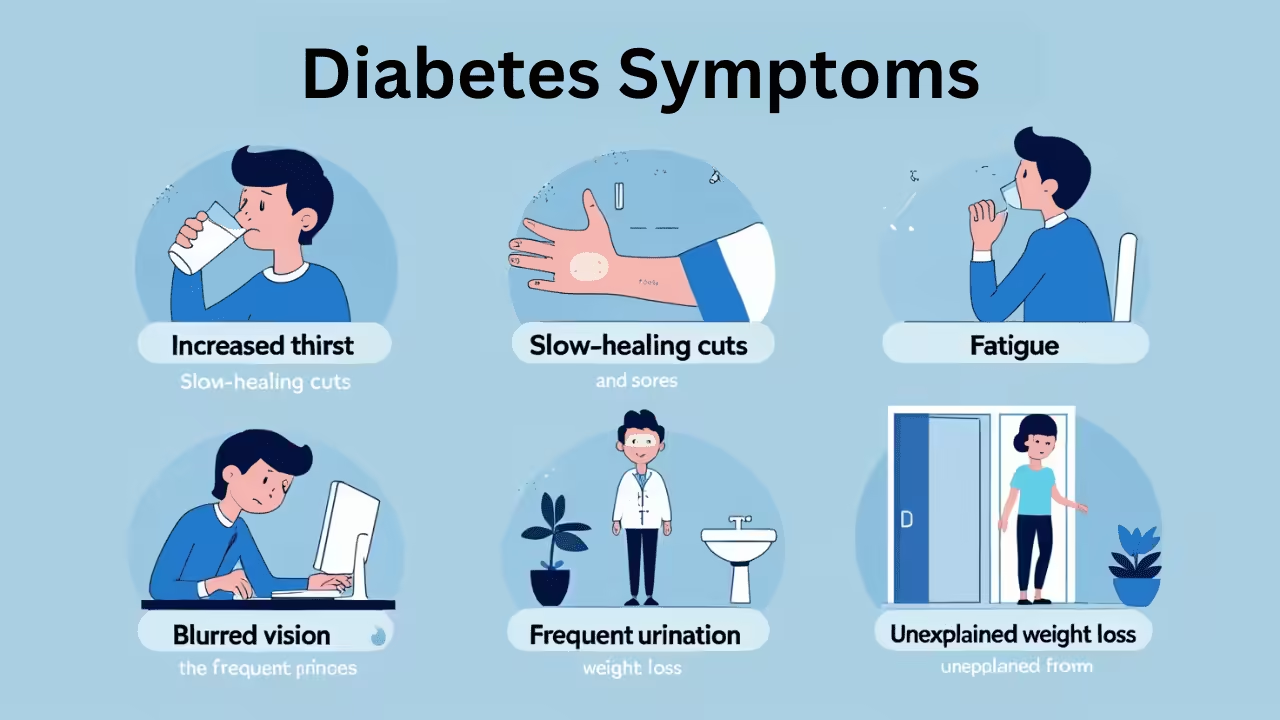
What Is Diabetes: Understanding Causes, Types, and Management Understanding Diabetes: A Brief Overview Diabetes is a chronic condition characterized by high levels of sugar in the blood. It occurs when the body either does not produce enough insulin (a hormone that regulates blood sugar) or cannot effectively use the insulin it produces. This results in